By Amanda A. Foster, Christopher J. Daly and David M. Jacobs
A person’s transition of care from hospital to home or another healthcare facility can be stressful for everyone involved.
However, when there is poor communication within the healthcare system, stress levels can multiply and avoidable medical errors and preventable hospital readmissions may occur.
The following is an interview with a local caregiver, Elena, during her mother’s care transition experience.
It’s provided in detail for the reader to fully appreciate Elena’s experience and challenges.
By the end, you may discover, unfortunately, a common disadvantage of our healthcare system and how caregivers play a key role in decreasing the chances of error during care transitions.
“Overall, the healthcare system in this country has so many cracks it’s pathetic,” Elena said.
She described a series of communication breakdowns in the healthcare system during her mother’s care and transition between healthcare facilities. The first major one occurred when the initial hospital was insistent on discharging her mother despite new complaints of stroke-like symptoms.
After Elena advocated, the hospital halted the discharge, ran additional tests and determined her mother had indeed suffered a stroke.
“If I didn’t speak up to the discharge nurse and scream for a doctor, my mom could have suffered another stroke and died on me in the car on the way home,” Elena said.
Her mother was in serious condition and needed immediate transport by ambulance to a heart-focused hospital. She was further aggravated when the healthcare system didn’t appear concerned about how long it was taking for the ambulance to arrive.
Elena was told that her mother may not survive the next hour—it took more than an hour for the ambulance to finally arrive. Before departing, Elena communicated her mother’s life-sustaining treatment decisions to the paramedics. If Elena had not spoken up then, her mother may not have received the proper treatment.
Upon arriving at the heart-focused hospital, Elena discovered that her mother’s life-sustaining treatment decisions were again not provided, nor updated, in the transfer process.
She sat with her mother, who was in critical condition, and explained her wishes to a healthcare professional for a third time. Once the hospital stabilized Elena’s mother, she was transferred to an observation unit awaiting a heart procedure.
As the highly anticipated procedure date got closer, her mother’s healthcare team decided to delay it a few days due to fluid build-up. Elena went home since the surgery was no longer happening the next day.
However, at 6 the next morning, Elena’s mother called and said they decided to do the procedure after all and were immediately taking her to surgery.
It took Elena more than two hours to receive a correct answer on her mother’s situation and finally locate her within the hospital. By this time, her mother had already gone into surgery and all she could do was wait; never having the opportunity to offer her mother comfort or hold her hand before surgery.
Elena was brought to joyful tears when the doctor finally came out of surgery and explained that everything went well.
During the recovery, 48 hours later, Elena was provided an information packet on rehab facilities and told to “do her research” on where she would like her mother to be transferred. The social worker representative wasn’t even aware the hospital had an acute medical rehabilitation unit just two floors above the floor where Elena’s mother was recovering.
Elena had to remind them and said that was her preference for continuum of care due to its proximity and ease of access to the full scope of critical medical resources at the hospital.
“You shouldn’t have to scream and act out of character to get results,” Elena said.
This situation highlights the critical cracks in communication within the healthcare system when transitioning between healthcare facilities.
Elena is a retired medical and scientific illustrator and graphic designer within a hospital-based creative services department and still had to face many challenges navigating her mother’s situation. It’s upsetting to think about what someone not familiar with the healthcare system may experience.
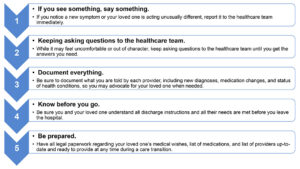
We can all agree that things need to change in the healthcare system. But the question is: “How?” One method is to speak up and make your voices heard. Whether by participating in research projects, completing healthcare system surveys, contacting legislators or speaking out in the media, caregiver and patient voices need to be heard. Power and change come with unity and numbers. We all must remember that any one of us could go through similar experiences as Elena faced or her mother endured. We need to start making a difference now.
Amanda A. Foster is a postdoctoral clinical research fellow in the department of pharmacy practice at University at Buffalo School of Pharmacy and Pharmaceutical Sciences; Christopher J. Daly is clinical assistant professor in the department of pharmacy practice at University at Buffalo School of Pharmacy and Pharmaceutical Sciences; and David M. Jacobs, Ph.D., is an assistant professor in the department of pharmacy practice at University at Buffalo School of Pharmacy and Pharmaceutical Sciences.
